U of R Stories

Record Turnout at Careers Day 2025: U of R Connects Students with Future Careers
Recent Posts
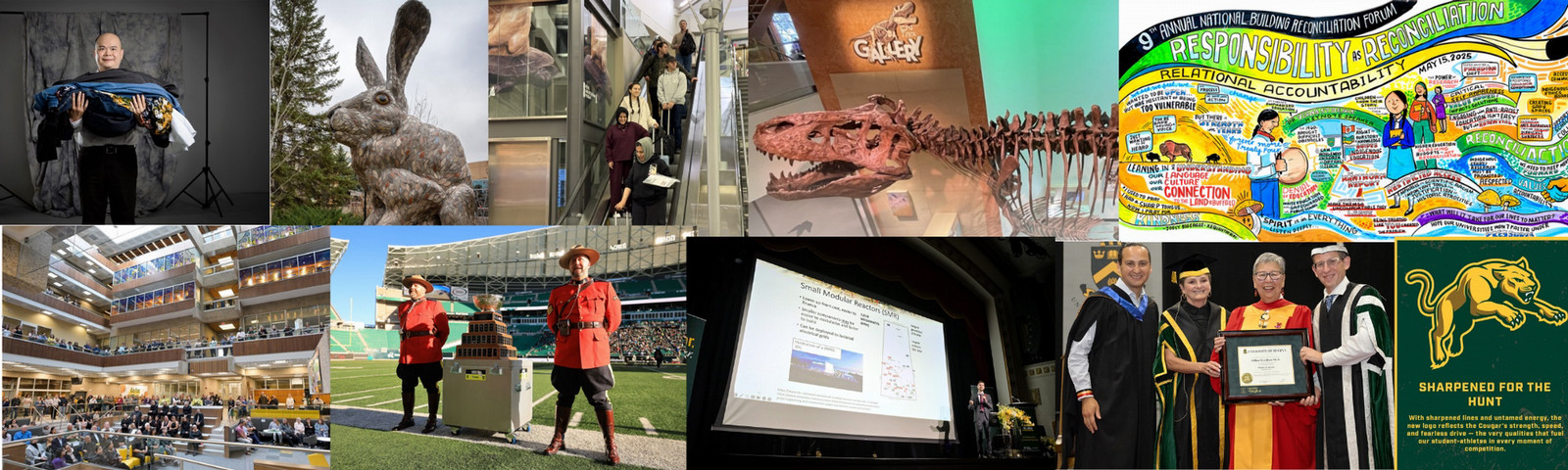
Year in Review: Top U of R Stories from 2025
Check out the exciting and transformative ways that our campus community drove change, celebrated milestones, and forged stronger partnerships in...
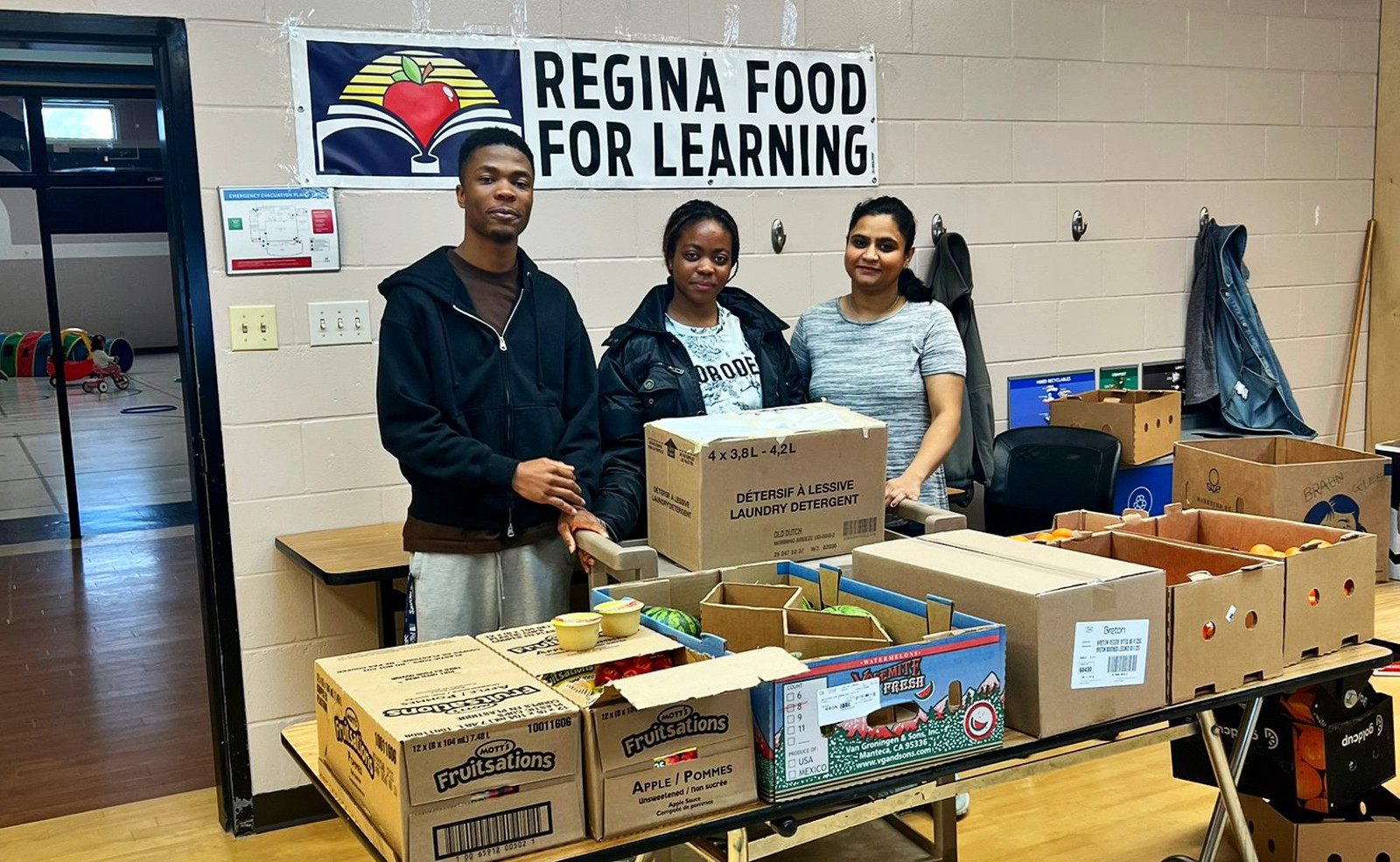
U of R Students in the Spirit of Giving All Year Long
Sometimes the most meaningful gifts are not wrapped, they are baked, delivered, and shared from the heart.
Record Turnout at Careers Day 2025: U of R Connects Students with Future Careers
More than 100 employers met with U of R students at Careers Day 2025, the largest career networking event in recent campus history.
Volunteers Power “Best-Ever” Vanier Cup Weekend in Regina
Once again, Saskatchewan – and Regina – proved why they are known as the volunteer capital of Canada as hundreds stepped up to help...
Andrew Coyne on the Crisis of Trust: The Minifie Lecture Returns to U of R
After a five-year pause, the Minifie Lecture returned to a packed house, featuring Globe and Mail columnist Andrew Coyne on the future of truth in...
At Canadian Western Agribition, U Of R Science Takes the Bull by the Horns
U of R’s Biology Department showcased science in action at Agribition, highlighting research that supports farmers in protecting their herds,...
More Than Ramps: University of Regina Launches Landmark Accessibility Plan
Shaped by hundreds of community voices, the new plan charts a course toward a campus culture where accessibility is a shared responsibility and a...
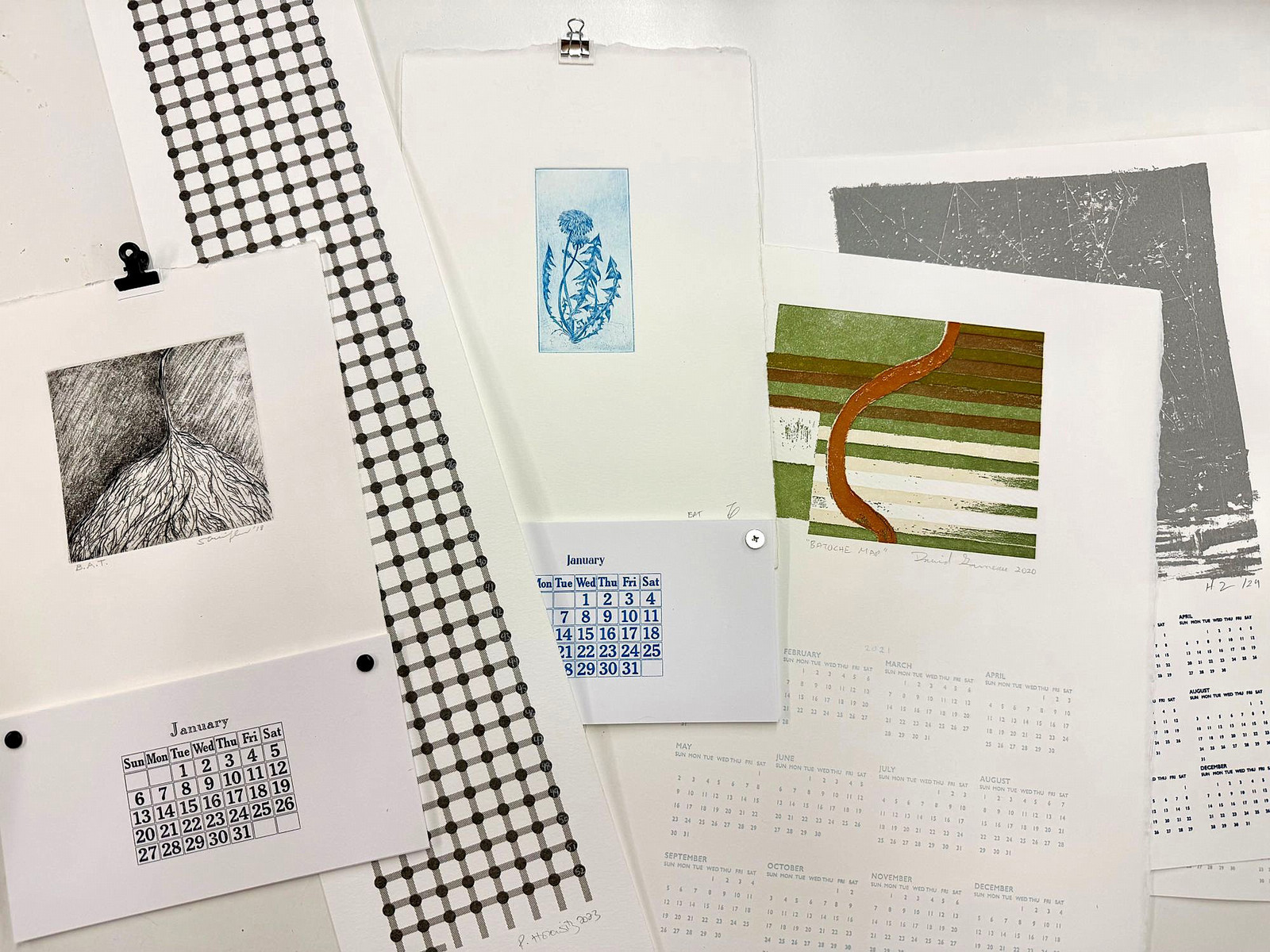
The Forty Project: Art Sustaining Art at the U of R
Discover how a handcrafted calendar helps fund students' access to professional printmaking at the University of Regina.
University of Regina named among world’s best in five subject areas
U of R earns global recognition with five academic subject areas ranked among the world’s best.
U of Regina Shines as Host of the 60th Vanier Cup
Even the weather cooperated as the 60th Vanier Cup was played in Regina under clear skies and above-average temperatures.